 In recent years, there has been a concerning rise in cancer incidence and mortality among individuals aged 15–39. Notably, colorectal cancer (CRC) has shown an uptick in cases among those under 50, both in the US and globally. This underscores the urgent need for preventive measures to mitigate cancer risks and elevate awareness.
In recent years, there has been a concerning rise in cancer incidence and mortality among individuals aged 15–39. Notably, colorectal cancer (CRC) has shown an uptick in cases among those under 50, both in the US and globally. This underscores the urgent need for preventive measures to mitigate cancer risks and elevate awareness.
While it might be perplexing to see the unexpected rise in cancer among the younger population, considering that traditionally cancer primarily affects older adults, the reasons behind this trend are complex and fascinating. Let’s delve into this in simpler terms.
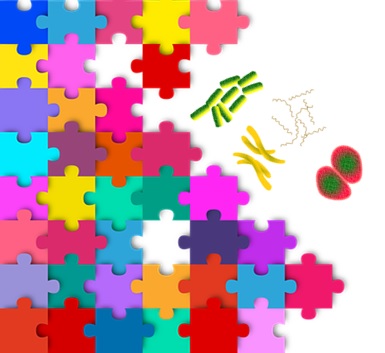
Cancer is caused by mutation, i.e., a permanent change in the DNA sequence of an organism. Mutations can result from damage to DNA and errors in DNA repair.
Imagine DNA as a blueprint for building a magnificent LEGO castle. Each LEGO brick represents a specific unit of DNA called a “base pair”. DNA damage is like the LEGO bricks get chipped or break due to various factors, DNA repair by enzymes works as repair crews identify damaged bricks and replace them with new ones. When the damage is too severe or the repair crew is overwhelmed, the building plan (DNA) can be disrupted and structural crises in the castle (cell malfunctions) take place.
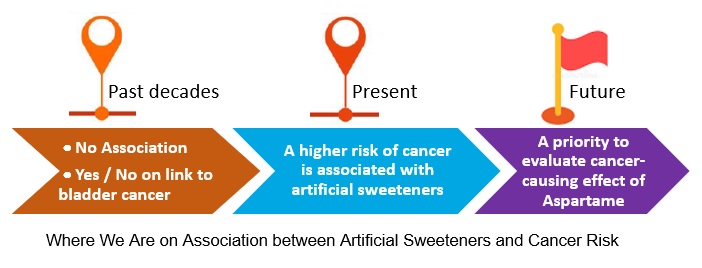
We know that most of cancer risk in aging adults can be attributed to randomly acquired mutations in proliferating tissues or susceptible cell types. In contrast, cancers in younger individuals result from the presence of genetic predisposition or the exposure to carcinogens (cancer-causing agents) or both, which all impact DNA damage and repair, genomic integrity, and then accelerate cancer growth in a young body.
To illustrate further, its origins have three key elements: inherited genetic predisposition, environmental carcinogens (including cancer-causing viruses), and developmental mutations—the latter can vary greatly depending on mutational rates in various cell types. Importantly, the interplay between each element and among these factors can also contribute to the variation in cancer risk among different cells, tissues and age groups.
Colon cancer is not the only type of cancer with a high prevalence in young people. Other cancers include:
- oropharyngeal cancers (more in adolescent and young cancer survivors),
- breast cancer,
- cervical cancer,
- skin cancer, melanoma and
- pancreatic cancer – its genomic feature distinctly involves the well-known tumor genes (including breast cancer’s BRCA1 and BRCA2).
I’d like to highlight some harmful environmental factors more relevant to young people, and mostly also apply to a broader population.
- Traumatic brain injury (resulting from car accidents, sports, falls, bast injuries but leading to long-term chronic neuro-inflammation in the brain and link to CNS tumors)
- Oncogenic pathogens or carcinogenic viruses – such as Infections by the human papilloma virus (HPV), causing cervical and oropharynx cancers; Infections by the Epstein-Barr virus (EBV), causing lymphomas and nasopharyngeal cancer; Merkel cell polyomavirus, causing Merkel cell carcinomas; Human T-cell lymphotropic virus, causing leukemias; and Fusobacterium, associated with colorectal cancer.
- Hazard environmental exposures – Sunlight/UV damage, causing skin cancer; air-borne radon or tobacco smoke, or air-borne asbestos, causing lung cancer.
- E-cigarettes – potential risk for oral cancer
- Food-borne pre-carcinogens and/or carcinogens: generated by chemical or physical food processing, including N-nitroso compounds (NOCs), polycyclic aromatic hydrocarbons (PAHs), heterocyclic aromatic amines (HCAs), and acrylamide. Moreover, some fungi- and plant-derived substances pose a cancerous potential. Their mechanisms of action and relevance to human biology can be classified as either genotoxic (DNA-reactive) or epigenetic (effects other than DNA reactivity).
It’s essential to remember that adolescents and young adults diagnosed with cancer face a risk for early death. This risk, influenced by factors such as age at diagnosis, race, ethnicity, lower socioeconomic status and cancer type, is multifaced and requires adequate healthcare with careful monitoring.
Next, let’s move to colon cancer, especially early-onset CRC, with an emphasis on risk factors.
Modifiable risk factors
These include obesity, type-2 diabetes, heavy sugar and red meat diet, physical inactivity, smoking, high alcohol consumption, inflammatory bowel disease (IBD), and frequent antibiotic use.
Non-modifiable risk factors
Particularly for early-onset CRC, being male, black or Asian, having IBD, or a family history of CRC are among non-modifiable risks.
Based on recent scientific evidence, early-onset CRC is associated with a genetic predisposition, mainly attributed to sporadic mutations in some genes (e.g., APC, KRAS, BRAF, TP53) that trigger uncontrolled cell growth and subsequent tumor formation.
However, one overlooked group is individuals younger than 50 years (<50 years) who do not usually undergo screening if they are at average-risk (defined as those without a personal or family history of CRC, without a personal history of IBD). Currently, there are little data regarding risk factors for CRC at average-risk young adults who are also asymptomatic.
Act to lower cancer risk
Armed with a comprehensive awareness and an inner-warrior mindset, act swiftly in the specific domains to impede or prevent cancer development within your young body.
- Live a healthy lifestyle. Eat a plant-based diet, stay active, avoid smoking, limit alcohol, and practice sun-safety.
- Maintain a healthy weight.
- Get screened for early detection.
- Get cancer risk assessment and genetic counseling. (for high-risk individuals)
- Get the HPV vaccination. Protect yourself from sexually transmitted infections.
Finally, cancer in young people disrupt crucial life stages such as education, career development and family planning. Early diagnoses can have long-term consequences in every aspect of individual’s well-being. Furthermore, the rising cancer burden in young people poses a significant public health challenge. Thus, the unexpected vulnerability in young people demands our attention and dedication to this troubling shift.
Image credit: Matt Cole, Mis wanto at Vecteezy