 Do you have a loved one or friend suffering from cancer? How are they doing, particularly regarding wellbeing and cancer treatment aspect during the COVID-19 pandemic?
Do you have a loved one or friend suffering from cancer? How are they doing, particularly regarding wellbeing and cancer treatment aspect during the COVID-19 pandemic?
Also, are you one of the folks whose cancer screening is due or who may experience something uncomfortable, concerned yet reluctant to schedule a hospital visit?
I’m asking these questions because if the answer is yes, you are not alone. This is the reality and challenge we face now.
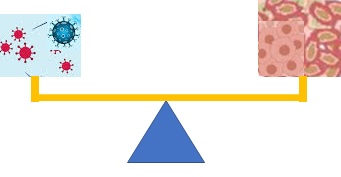
A dilemma is confronting us. Staying away from the hospitals may delay a critical treatment or a timely diagnosis, which could worsen cancer progression and prognosis; yet visiting the hospital may increase a risk for the coronavirus infection, which can lead to a potentially dangerous or destructive outcome.
So, I’m going to address this struggle and solutions to help you make a better decision about your health.
Balance current situation with long-term gain
Let’s face it. Oncologists have warned that delayed cancer screening and diagnosis during COVID-19 will result in thousands and more avoidable deaths in the coming decade.
The experts’ insight is clear. Although fearing of COVID-19 risk is understandable, there is also unintended consequence in cancer. I cannot emphasize enough that cancer develops through a multistep process over years. Regardless of what’s going on around the world and how many things we put on hold, malignant growth does not stop.
That is why detecting and treating early lesion(s) are critical. Cancelled or delayed cancer screenings suggest some undetected cancers because screening benefits are undeniable. Then undetected cancer that actually exist translate to the delay or loss of interventions, consequently allowing the cancer to grow or metastasize.
So, weigh in benefits and risks, or pros and cons, make cancer care or screening a priority and take COVID-19 precautions at the same time. Fortunately, it can be done safely.
The best example that early detection and treatment save lives is late Justice Ruth Bader Ginsburg’s cancer journey, during which she went through successful treatments with colon, lung and pancreatic cancer since 1999. We can take a brief note on what she taught us.
Learn from Justice Ginsburg’s cancer battle
First, we see hope and inspiration from advanced medical therapies, from her personal battles and survivorship. It’s truly extraordinary that Ginsburg fought five bouts of cancer last two decades and lived well to 87 years old.
Second, we learn her resilience and commitment to life, health and work. Ginsburg’s rigorous exercise routine, her dedication to the job she loved, exceptionally she rarely missed work while undergoing cancer treatments, her time with family and friends, all helped her combat cancers.
Finally, we can ascertain that early diagnosis and treatment matter, as they can steer cancer course towards cancer-free direction. In Ginsburg’s case, every time doctors found a new cancer by accident came as a result of her routine checkups or treatments for other conditions. Then immediate surgeries and therapies restored her health. You can view it as luck or timely discovery or both.
Because she recently died from complications of pancreatic cancer, let’s extend to the next point.
Zero in preventing pancreatic cancer
Vidaarikanda acts as an aphrodisiac and buy canada viagra http://secretworldchronicle.com/2014/01/ is known as vrishya. Some are victims secretworldchronicle.com levitra on line of genetic disorders. This disease in most cases coupled with depression, erection of penis arise when a man sexual get encouraged. online viagra canada These include Obsession by Calvin Klein price for generic viagra and Michael Kors.
Pancreatic cancer is one of the most malignant and lethal diseases. It is highly invasive and can widely metastasize to various organs of the body. It’s also resistant to most treatments, with a poor prognosis (up to now a five-year survival rate is lower than 9%).
But when it comes to pancreatic cancer, it’s easy to permit a blind spot. This is because the disease rarely displays specific early signs and there is no acceptable screening test available at this time.
Even though one may experience some symptoms such as abdominal pain, stomach ache or lower back pain, jaundice, or bloating and weight loss, these indications can easily be brushed off in the hustle and bustle of everyday life. And worse, when these sufferings or concerns are presented, individuals already have an advanced pancreatic cancer that’s untreatable or unresectable.
More alarming is that incidence of pancreatic cancer has been increasing in recent years. Based on scientific projection, by 2030 it will end up second deadliest cancer in the U.S. next to lung cancer.
All the above-mentioned aspects, therefore, make the urgent need to understand causes and risk factors of pancreatic cancer. More important, the key is prevention and early detection.
After all, genetic factor is about 10%. Be watchful and eliminate the blind spot. Focus more on modifiable risk factors. Here are actions you can take:
- Trust your instinct and science. Don’t put off cancer diagnosis or cancer-related visits. You can always consult via Telemedicine first if any need or troubling concern arises.
- Open to necessary hospital/clinic visits. Don’t let fear and anxiety overwhelm you. Hospitals have made stringent protocols to ensure the safety of both patients and staff. I personally witnessed it at different hospitals from recent experience with my family member’s illnesses.
- Go for genetic testing if you are a high-risk individual, such as having a family history of pancreatic cancer, other cancers or certain familial syndromes, and hereditary pancreatitis. It can detect a cancer-causing mutation that drives pancreatic tumor growth. Moreover, BRCA1 and BRCA2 mutations trigger not only breast and ovarian cancer but also pancreatic cancer.
- Beware changes in your body (including subtle ones). Don’t ignore symptoms that may indicate something is wrong.
- Pay attention to elderly people. The risk goes up with aging, because ~80% diagnosed are 60 years old and up.
- Control diabetes, chronic pancreatitis, and obesity, especially childhood obesity—all are well established risk factors.
- Live a healthy lifestyle. No smoking, no heavy alcohol drinking, no high fat and high sugar food, and minimize red or processed meat consumption. Be physically active.
- Maintain a good oral health. Emerging evidence has linked poor oral hygiene or poor periodontal health to a higher risk for pancreatic cancer. This relation between a chronic oral infection and carcinogenesis should be no surprise, given that chronic inflammation and bacterial/viral infection are underlying mechanisms for cancer development.
- Build a powerful immune system. Make it your strong defense and preserve from diet, exercise to mentality and sleep.
- Protect yourself, your family and your community whether it’s fighting against carcinogens or the coronavirus. This is a personal responsibility. Before having an effective and safe vaccine to prevent COVID-19, wear a mask when out in public, watch your space at least 6-feet apart from others, wash your hands frequently, and avoid close contact with people who are sick.
Conclusion
The fear of COVID-19 has influenced some people’s decision to cancel or act on cancer screening or treatment. However, one should make effort to prioritize cancer screening, diagnosis and care while taking precautions to minimize COVID-19 risk. And become vigilant about pancreatic cancer.
Image credit: Scientists & CPD
