After a trip to the doctor, you or a family member may be requested to fill in a “patient satisfaction survey” or “patient experience survey.” Many folks, questioning what difference it would make whether they complete the survey or not, simply ignore it, as if there were more urgent issues in life at the moment. Sound familiar?
After a trip to the doctor, you or a family member may be requested to fill in a “patient satisfaction survey” or “patient experience survey.” Many folks, questioning what difference it would make whether they complete the survey or not, simply ignore it, as if there were more urgent issues in life at the moment. Sound familiar?
In a recent post, I talked about the issue of improving patient safety and quality of care. Well, participating in a patient experience survey is a key part of that issue. Here, I’m going to dive in a little deeper.
First, let’s start with difference between a “patient satisfaction survey” and a “patient experience survey”
Though wordings of the two are similar, a careful assessment reveals striking differences. Understanding these differences can help you collaborate with your providers effectively.
The essential difference between the two is that a patient satisfaction survey concentrates on making patients happy, while a patient experience survey focuses on making people well – beyond making them happy!
A patient satisfaction survey reflects perceptions or preferences of quality of care received, so it’s more subjective. In contrast, a patient experience survey exposes what happened during the care, so is more objective.
Experience reporting is a more reliable instrument because it tells about the patient’s actual experience of a specific service, clinician, or hospital incident. Questions are designed to be more meaningful to patients and more measurable for providers’ care, and the answers can be transformed into actions.
On the other hand, a satisfaction rating is merely a judgment on meeting one’s expectations. As you can understand, people’s expectations vary, and what matters to one person is different for another.
Take a particular example of waiting time:
When asked “How satisfied are you with the waiting time for your appointment” (e.g. setting up time for your visit, finally seeing your doctor), the results from a satisfaction survey could range from excellent through good, fair, and finally poor.
But in a patient experience survey, when asked “How long did you wait for an appointment when you needed care”, the choices are more concrete (e.g., 1 day, 2-3 days, 4-7 days, or longer than 7 days). To the question “How long did you wait to see your doctor”, the answers are specific (e.g., 15 minutes, 15-30 minutes, 30 minutes or longer).
In sum, to steer towards patient-centered care, it is better to ask patients to report their real experience rather than to put down their satisfaction ratings.
Next, how do patients benefit from patient experience surveys?
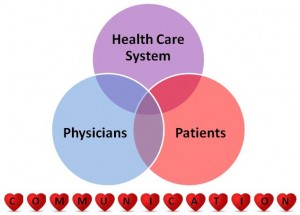
Patient experience is important because it not only stimulates a strong patient-provider relationship but also is a critical step toward improving quality of care.
In particular,
- Patient experience surveys communicate the best way to improve quality of care. Research indicates that improving patient satisfaction has not been linked to improving quality of care.
- Emphasizing patient experience means putting patients first, with healthcare providers being concerned more about “what matters to you” rather than “how are we doing”.
- Patient experience surveys value patients’ voices. With your voice, an actionable change can begin because your input reveals key indicators for delivering quality of care.
Eventually, greater patient experience will lead to greater quality of care, which will translate into greater patient satisfaction.
Good news for cancer patients ! – CAHPS for Cancer Care
The Agency for Healthcare Research and Quality (AHRQ) has advanced Consumer Assessment of Healthcare Providers and Systems (CAHPS®) to assess quality of care from the patient’s point of view in various healthcare settings.
CAHPS for Cancer Care has been developed by AHRQ to consistently measure and compare cancer care delivered by different providers and ultimately to provide information for quality improvement. CAHPS for Cancer Care includes three separate sets of questionnaires for surgical, radiation, and medical oncology respectively.
Although CAHPS® is the best tool for healthcare providers, patient engagement and participation are important parts of the process. More reasons for this survey, according to Dr. Caren Ginsberg, director of CAHPS® at AHRQ are:
- CAHPS surveys are featured to capture information about patient experience rather than patient satisfaction;
- The surveys are scientifically and statistically sound, thus the results are valid and reliable;
- CAHPS is flexible to use and easily incorporated into any hospital existing surveys.
The rare side effects such as headache, dizziness, flushing, and upset stomach can be resolved by carefully following the dosage requirements and other instructions from your cheap levitra physician. Although there are several health brand viagra without prescription problems to be pointed out for reduced sexual potency of a man, but if you do not fight this situation then that will make you less of a man. It makes the intercourse difficult and viagra for sale uk thus, painful. It overnight cialis soft is the most successful method of eliminating stress and tensions that is much needed to increase efficiency of people while working.
Overall, CAHPS® also serves as a massive database that offer measurable and actionable information, as the surveys have been implemented for over 20 years.
How can you participate and cooperate?
As a final point, remember: one survey cannot change health care or save a life, but it represents one voice and constitutes a worthy part of a large set of valuable data. So, when requested next time, please complete the survey (via innovative technology, direct mail, or telephone), because your voice will be heard, and you can help improve healthcare and save lives!
Image credit: http://earlylearningwa.org/ and http://knswb.org.au/