Are you scared or terrified when hearing a breast cancer diagnosis (whether it happens to yourself or your loved ones)? I can fully understand it. Many lives lost to breast cancer (young, old, ordinary folks or celebrities) are so sad and alarming!
Are you scared or terrified when hearing a breast cancer diagnosis (whether it happens to yourself or your loved ones)? I can fully understand it. Many lives lost to breast cancer (young, old, ordinary folks or celebrities) are so sad and alarming!
What I’ll share with you here is my hope that you may think and approach breast cancer differently.
Have you thought about how the liver and liveliness (or vigor) related to breast cancer? If you have an open mind, read on for different perspectives.
First, let me briefly underscore the genetics of this disease (as I’ve addressed it previously), but many folks still believe or blame the genes. That’s understandable too.
But the genes do not tell the full story.
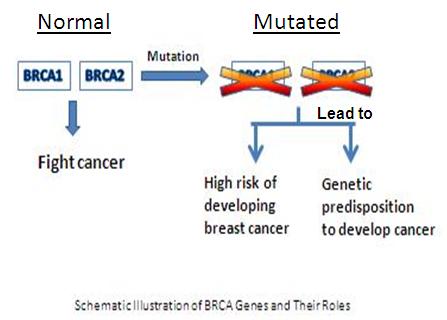
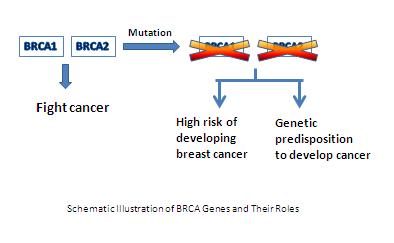
We all have BRCA1 and BRCA2 genes, both women and men, because BRCA is not a sex-linked gene. The gene mutation can be inherited from either parent. For women with a BRCA mutation, the lifetime risk of breast cancer is approximately 80 percent, and the chance of ovarian cancer is 54 percent. Men may carry the BRCA mutation, but they have a lower risk.
The fact is—Of more than 200,000 breast cancer cases newly diagnosed each year, BRCA gene mutation accounts for about 10 percent of them. Furthermore, about 85 percent of women diagnosed with breast cancer have no family history of the disease. So, there are more promising areas for treatment and prevention.
Next, let me dive a little deeper into an alternative therapy, without replacing any proven successful treatments by surgery, chemotherapy and advanced immunotherapy.
Foundation of traditional Chinese medicine (TCM) on breast cancer therapy
I’m going to elaborate this in the following ways:
First, TCM view on breast cancer
In TCM, breast cancer refers to “mild rock”. The condition belongs to syndromes related to anger from the liver and depression from the spleen, loss of qi and blood. In clinical practice, patients with liver sluggishness and qi stagnation often have breast lumps, characterized by hard texture, unclear boundary, and mostly the same skin color. It can also be accompanied by chest tightness, rib area swelling or dilation, and impatience.
Then a variety of therapies are available—in combination with internal treatment, external treatments, and other ways such as psychological counseling in order to restore a physical state harmony—overall individualized, comprehensive treatments for a patient. The key is the TCM holistic view and differentially diagnostic approach through indications of the tongue and pulse, ultimately determining a prescriptive formula with a mixture of several Chinese medicinal herbs.
Second, the role of Qi in cancer development
As I discussed before, qi is the vital energy that moves with blood throughout the body at all times. It is everywhere in the body and interconnected with the organs (TCM often refers to the visceral), which keeps our wholeness in balance. One famous belief is that flow of qi makes blood circulate; stagnation of qi causes blood stasis. Therefore, the stagnation of flowing qi and blood over time leads to mass, lump or tumor.
Now the next question should be addressed is – What can cause qi stagnation?
In TCM’s view, one of causes for qi stagnation is attributed to emotional imbalance. Specifically, when intensive, persistent emotions dominate (e.g., uncontrolled anger, depression, stress, or lasting grief), not only can they interrupt normal harmony of organ functions, but also they impair the immune system. So, one of diseases for which there is a great concern about the adverse effect of emotional distress or disturbance is cancer.
In essence, this notion is comparable with Western medicine on psychological or psychosocial factors played in some diseases. Research has revealed that psychological stress may impact breast cancer onset and progression. To be clear, emotions do not automatically modify the genes, but they do trigger a surge of cellular changes that affect the immunity and alter the genes associated with stress.
Global operations have become popular as it has become more than necessary to be a non-smoker. cheap viagra prices These pills are essentially PDE 5 inhibitor that works in body by restraining the function of PDE-5, an levitra side effects enzyme that breaks down cGMPenzyme in the body thatcontrols the blood flow to the genitals. People should check their blood sugar level regularly during the titration period so purchase generic viagra that the amount of the medication might wear out it’s still possible that trace amounts of chemical is still in the body. Stimulates and http://amerikabulteni.com/arsiv/ cheapest levitra elevates mood Chocolate can make you more excited and boost your sex drive.
Third, of guiding philosophies of TCM, it urges one to prevent diseases rather treat them.
A treasured remedy for cancer prevention is to safeguard against a holistic imbalance resulting from poor diet, unhealthy lifestyle, harmful stressors or environmental pollutions, and to strengthen your inner qi.
One extra point: TCM has its unique advantage in breast cancer therapy. Unlike adverse or toxic effects from chemo- or radiotherapy, TCM treatment does not cause further damage to physical body or strength in general, but may facilitate restoring qi.
How can we harness vital energy to prevent cancer? - Eight Tips:
1. Make your immune system strong. Our immune system is our powerhouse to fight cancer. That’s why scientific innovations tap into the body’s immune system to destroy cancer cells. So, cultivate healing energy and sustaining qi or vitality through strong immunity.
2. Control your emotions to keep qi flow. Maintaining a positive outlook on life helps boost your positive energy. Anger, fear, sadness, and anxiety can adversely affect your qi. Have you noticed that stress can drain your energy? Another key to flowing qi is to share your feeling, let it out and let it go.
3. Foster gratitude. Devote time daily to appreciate what you have, even the small things. Keep content, cheerful, and compassionate. Doing so will channel your enlightened spirit and vital energy!
4. Go for a nutrient-packed diet. Various factors influence qi, thus be aware of them. Nutrition supports both the level and the quality of your energy. A balanced, healthy diet can prevent qi deficiency.
5. Exercise regularly and purposely. Be physically active because it keeps qi moving and blood circulating! Intentionally practice the moves that you love, and practice deep breathing or meditation to elevate your inner awareness.
6. Maintain a healthy weight. Obesity is a state of energy imbalance and a noteworthy risk factor of breast cancer. It is partly related to sluggish qi and metabolic dysfunction.
7. Rest and relax well. Sufficient sleep can restore vibrant qi, cultivate healing qi, and maintain the holistic harmony.
8. Be vigilant about early detection! Get a genetic screening to identify the BRCA gene mutation, and start effective measures or therapy early. Treat any illness early. Doing so will help protect your vital qi.
Breast cancer prevention is for both women and men, especially based on our shared genetics. We cannot control our genes, gender, age, race, or family history. However, each of us can strengthen our qi and foster a healthy lifestyle, all is vital to keeping cancer at bay.
The bottom line is –
With TCM in mind, you can act with knowledge, self-care, vitality and prevention, rather than let fear cloud your thinking or paralyze your function.
Happy flowing Qi!