 Cancer. The word itself can send shivers down your spine. How about pancreatic cancer? Consider these three facts:
Cancer. The word itself can send shivers down your spine. How about pancreatic cancer? Consider these three facts:
- A grim reality: Pancreatic cancer is a rare and deadly cancer. Estimated 66,440 people in the US will be diagnosed with and approximately 51,750 Americans will die of pancreatic cancer in 2024 (per American Cancer Society). Data also predicts the disease to become the second leading cause of cancer deaths by 2030.
- A growing concern: Pancreatic cancer diagnoses in young adults (under 45) are on the rise. As the incidence increases, it’s becoming a public health problem too.
- A glimmer of hope: Yes, let’s explore it as evolving breakthroughs combat this terrible disease!
First, let me briefly emphasize what makes pancreatic cancer extremely fatal. It is because of its key characteristics such as:
- Asymptomatic nature in early stages (if any signs, vague or nonspecific)
- No routine screening test available
- Invasive early and rapid spread
- Limited effective treatments
- Therapy-resistant, with high rate of recurrence
- Poor prognosis, with a 5-year survival rate about 10% or low long-term survival.
For the focus here, the most common type of pancreatic cancer (85% overwhelmingly) is pancreatic ductal adenocarcinoma (PDAC); its nature remains aggressive and multifaceted.
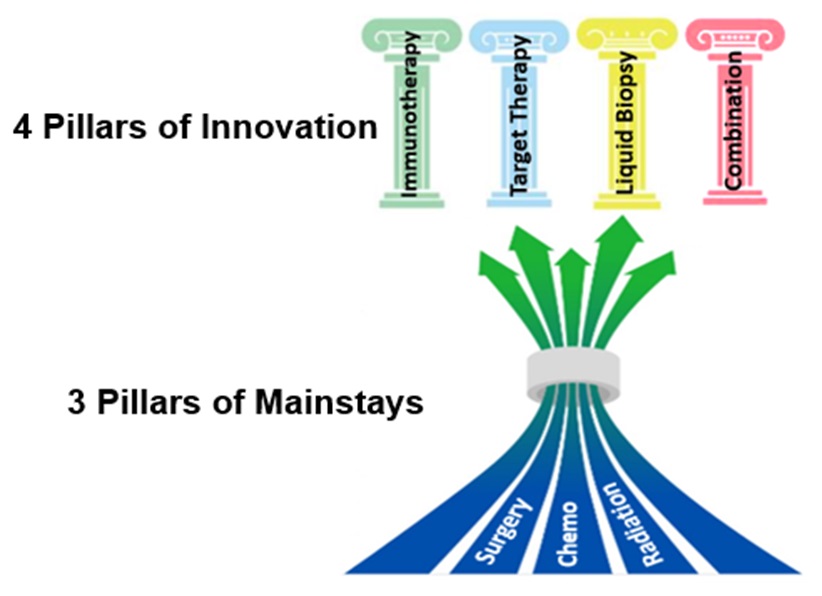
However, the mainstays for pancreatic cancer treatment are surgery, chemotherapy, and radiation therapy, which appear to reach a “bottleneck” status with unsatisfactory clinical results. Also sadly, most cancers have already metastasized at the time of diagnosis.
Despite its complexity, genetic research and scientists’ unwavering effort have propelled discoveries!
A hallmark of pancreatic cancer is KRAS mutation. KRAS is a tumor-promoting gene, and mutated in ~95% of pancreatic cancer patients. Studies indicate that KRAS mutation likely initiates human pancreatic cancer, and drives tumor growth and progression. Even so, targeting KRAS through pharmacological interventions—especially with single agent inhibitors in the past—has confronted an “undruggable” challenge.
Yet, researchers are unlocking new opportunities in various paths, with transformed treatments encompassing but not limited to:
- Targeted therapy: Innovative therapies—such as the use of siRNAs (small interfering RNA) through nano-delivery, anticancer vaccine, and immune T-cell therapy—are driven against KRAS mutation. Additionally, a subgroup of pancreatic patients harboring BRCA1/2 mutation can benefit from platinum-based chemotherapy and Olaparib (a PARP inhibitor). Next-generation sequencing technology will facilitate genomic mapping of cancer cells to identify more treatment targets.
- Immunotherapy: In the past, most pancreatic cancer didn’t respond to immunotherapy, likely attributed to its immuno-suppressive tumor microenvironment that facilitates tumor escape from immunosurveillance. Now, studies and clinical trials are ongoing to alter tumor microenvironment, and make tumors active immunologically or cytotoxic T-cells respond.
- Liquid biopsy: This is an emerging, non-invasive, and less costly clinical tool to detect cancer biomarkers or “signatures” from blood circulating tumor DNA (ctDNA) or circulating tumor cells, etc. It shows promises for early detection, treatment precision and monitoring, and offers prognostic value in pancreatic cancer.
- Combined therapies: In addition to a targeting approach, combined drugs to simultaneously block multiple abnormal pathways in PDAC, or a combination of immuno- and chemotherapy, can also improve survival and/or quality of life in cancer patients.
Still today, early detection is crucial, because pancreatic cancer is curable at an earlier, localized, and surgically resectable stage.
If you experience persistent abdominal pain, unexplained loss of appetite or weight, or any concerning symptoms, don’t hesitate to see your doctor. For those with a hereditary risk, consult with oncologists to keep updated on helpful or applicable genetic development.
Finally, with a glimmer of light, a glimmer of joy for the positive impact on cancer patients, it also creates an urgent need for our awareness and actions. Spread words and modify lifestyle!
Image Credits: slidemodel.com; CancerPreventionDaily